In 1967 Dr. Christiaan Barnard performed the first heart transplant. Until that time, if someone's heart was taken out, they died. People were astounded to learn that not only was a man’s heart removed, but a non-beating donor heart put in, restarted, and he lived. Years of design efforts and testing resulted in a sophisticated invention that circulated blood and functioned as patients' lungs to bring them oxygen--the all-important "heart-lung" machine.
No doubt in the same hospital in 1967 was a brand-new mother. Her baby had just made a similar transition of survival on an exceedingly better "lung machine," but no reporters covered it. Although the first event was a great feat of human engineering, the second has never been explained by any natural process.
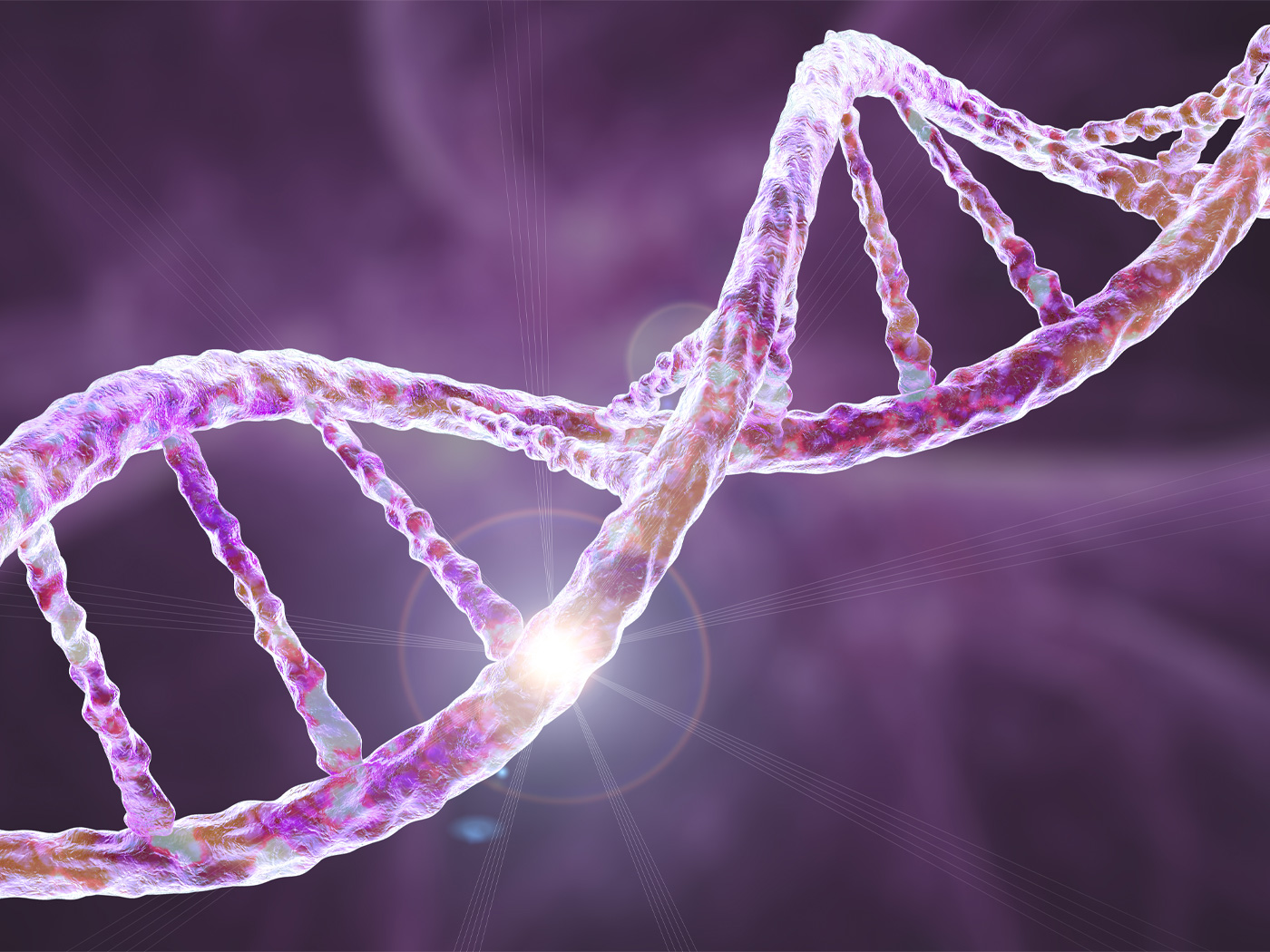
Childbirth is so common it is easy to overlook the fact that a baby thrives in a total water world for nine months--a world that is utterly impossible for any person to live in immediately after their very first breath. That feat is accomplished by the baby possessing--only in the womb--blood vessels with a different arrangement and structure than an adult's.
The Adult Circulatory Arrangement
In an adult human heart, the bottom two chambers, the ventricles, do most of the higher pressure pumping, pushing the blood through one-way valves away from the heart through arteries. The upper two, the atria (plural of "atrium"), receive blood under low pressure from veins and rapidly preload the ventricles by pushing blood into them, also through one-way valves.
The heart is also divided into left and right halves, separated by a solid wall of tissue called a septum. There are two circuits for blood flow from the heart: one to the lungs and back, and one to the body and back. The right heart starts blood on its circuit to the lungs, where less-oxygenated blood picks up a new load of oxygen. The left heart pumps freshly oxygenated blood at "normal" blood pressures (much higher than the right side) to the rest of the body.
In adults, oxygen-rich blood travels away from the heart through arteries under high pressures, and oxygen-poor blood flows toward the heart through veins under low pressure. Clearly, the heart and lungs are completely codependent in accomplishing the purpose of getting oxygen to all places in the body.
The Fetal Circulatory Arrangement
For a baby in the womb, almost everything about those vital functions is just the opposite for one important reason: the baby develops fully functional lungs that are yet inactive for oxygen exchange. Consequently, in order for a baby to survive, three major structural differences must exist that enable life in his temporary home.
First, the baby must have a substitute lung--a pretty tall order for even brilliant biomedical engineers. The placenta, a remarkable organ, has a brief existence, but it fulfills a myriad of vital functions--especially as the fetal lung and kidney. Second, the circuit to the lungs must be bypassed, so vessels must change to allow this temporary detour. (A new route that detours around a circuit is called a shunt.) Third, blood vessels must not only connect placenta to baby, but also inside from the point of attachment to normal vessels that lead to and from the heart. The umbilical cord meets the need for a placental-fetal connection, with one large-diameter vein and two smaller arteries. Inside the baby, these continue as the umbilical vein and umbilical arteries.
The umbilical vein carries oxygen-rich blood toward the heart. At a spot next to the liver, it connects to a large vein carrying less-oxygenated blood back to the heart. Interestingly, the two combined streams of blood do not tend to mix. It just happens that when they reach the right atrium, the more oxygenated blood stream is adjacent to a temporary opening in the septum, where it passes through to the left atrium because the blood pressure in the right side of baby's heart is higher than the left side--the opposite of the post-birth situation. The right heart still pumps blood to the lungs, but because the lungs have not yet expanded, the resistance to blood flow is very high and, therefore, the pressure is high. Some blood does make it to the right ventricle (about 10 percent) and flows through the lungs, which is the right amount to meet metabolic needs but not for oxygen-carrying purpose--which does not yet exist.
The temporary opening has a piece of septum tissue over it that is located in the left atrium. Thus, it acts like a "trap door" valve so that high pressure on the right side can push it open with each beat. In adults, it would make no sense for the artery carrying oxygen-poor blood to the lungs to connect by a big blood vessel to the artery carrying oxygen-rich blood (the aorta) to the body. But the baby does have this big connecting vessel in order to bypass the lungs and send oxygen-rich blood from the placenta to the body. Most of this blood travels to the part of the body with the highest oxygen demands--the growing brain.
So baby is content in the womb with temporary umbilical arteries and vein, a temporary opening in the septum, the temporary pulmonary artery-aorta shunt vessel, high pressure in the lungs and right side of the heart, and low pressure on the left side. With the onset of labor, culminating in delivery, that world is set to radically change. However, crucial mechanisms are built into the temporary structures that enable a safe transition out of the womb.
Vital Circulatory Changes Occurring at Birth
The umbilical cord vessels have features that respond to changes in quantities of oxygen dissolved in blood, stretching, substances commonly called adrenaline, and trauma. Obviously, during delivery and the severing of the cord all of these are present. The cord, which has an unusually strong muscle layer surrounding the vessels, reacts with a rapid and powerful constriction of the arteries and vein that is complete in less than a minute. This stops blood flow to and from the placenta, which has two effects. It greatly reduces the risk of either baby or mom losing a lot of blood and also causes an immediate drop in the amount of oxygen baby is getting.
Very sensitive sensors--inside certain blood vessels measuring carbon dioxide content, and also on the skin detecting temperature drops--stimulate the nervous system's breathing center. Under normal circumstances, increased carbon dioxide blood levels coupled with decreased body temperature after exiting the birth canal trigger an irresistible urge for baby to take a strong breath and inflate his lungs for the first time. The lungs have been prepared for this event by special cells producing a compound called surfactant, which significantly reduces the tension holding non-inflated lung tissues together--otherwise, forces required to open the lungs would be too high for almost all newborns to accomplish. Once inflated, pressures necessary to pump blood through the lungs drop 90 percent from their intra-womb high values.
Thus, pressure in the right side of the heart immediately drops well below the pressure in the left side. The "trap door" valve (actually two flaps of skin that neatly fold and interlock when pushed together) covering the septum's temporary opening in the left atrium is pressured shut. Cells begin to grow over the edges of the valve, fusing it to the septum. Less than a minute after birth, signals from baby's nervous system cause strong sphincter muscles to close off the umbilical vein where it attaches near the liver and also close off the temporary pulmonary artery-aorta shunt. (That large vessel permanently closes over the next one to two days.)
The baby's body has started all changes that continue through adulthood. During the next year, those internal umbilical vein and arteries transform from blood vessels into stabilizing ligaments. So in the one critical minute after delivery, the baby's body has initiated actual structural changes enabling it to survive in its radically different environment with all temporary vessels, shunts, and openings functionally closed in the first 30 minutes.
Conclusion
The reality of fetal to newborn circulatory changes is this: structures indispensable for life in the womb are incompatible with life out of it, and at birth all structures are rapidly reversed, resulting in the opposite effect on survival. In either case, if the offspring dies, evolution ends. Darwin wrote, "If it could be demonstrated that any complex organ existed which could not possibly have been formed by numerous, successive, slight modifications, my theory would absolutely break down."1
Consider it broken...if not a catastrophic failure. Why? Given that a transplanted heart living inside someone is truly an incredible achievement--at what level of accomplishment is getting a whole person to live inside another person? Absolutely incredible--which is what the Lord Jesus Christ is! As clearly seen, He creates, He directs, He provides, He cares--indeed, everything He does is beautiful beyond description.
Reference
- Darwin, C. 1859. On the Origin of Species. London: John Murray, Chapter VI, 189.
* Dr. Guliuzza is ICR's National Representative.
Cite this article: Guliuzza, R. 2009. Made in His Image: Baby's First Breath. Acts & Facts. 38 (12): 10-11.